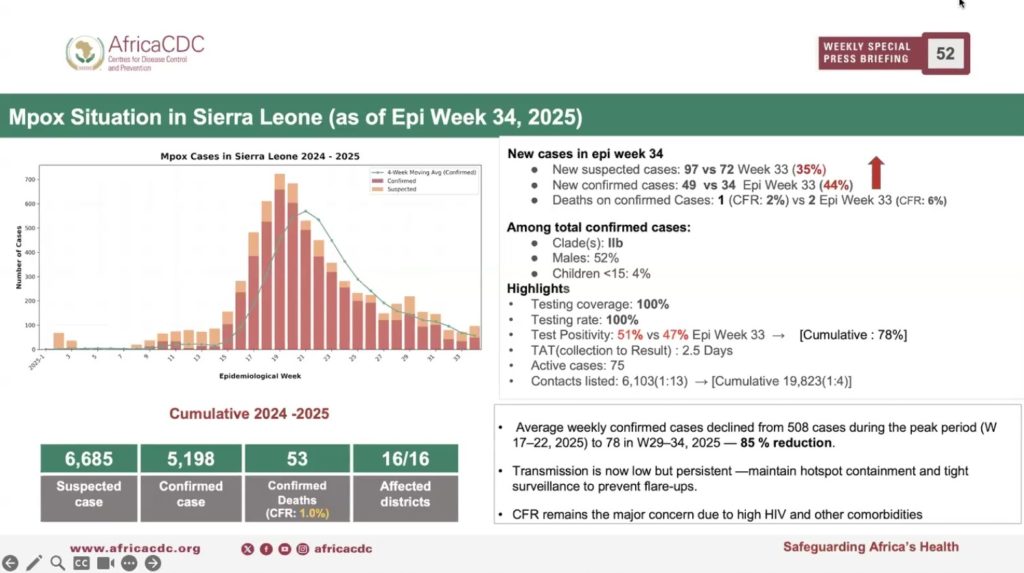
As Mpox cases continue to decline, one of the major remaining concerns for health authorities in some African countries is how to deal with high rate of fatalities.
In some countries, like Sierra Leone, the death rate becomes more worrisome due to its prevalence among people with comorbidities, like HIV.
Data from the Africa CDC shows that death from Mpox in Sierra Leone is the second highest – 53. It falls closely behind the Democratic Republic of Congo with the highest death toll of 121. These numbers are for the period January 2024 to September 4, 2025. Both are among the top four high burden Mpox countries, alongside Uganda, with 48 deaths and Burundi with just one death.
According to the Africa CDC data, the continent has recorded cumulative confirmed deaths of 250 in 29 countries since 2024. Majority of the deaths, 205 occurred this year, which has seen the worse Mpox epidemic so far, with a total of 29,720 cumulative confirmed cases.
The top four high burden countries collectively account for 89.2 percent of the total deaths (223). Among them, Sierra Leone has the highest case fatality rate of 1 percent, compared to 0.6 percent for Uganda, 0.41 percent for DRC and 0.02 percent for Burundi.
Other countries with high death rates of Mpox outside the high burden nations include Kenya, with 6 deaths, representing 1.5 percent case fatality rate.
This is one of reasons cited by Africa CDC’s Emergency Consultative Group (ECG) to advise against lifting of the Public Health Emergency of Continental Concern declared by the agency in August 2024.
“Mpox continues to remain a continental public health emergency of continental security as recommended by the ECG and accepted by our Director General, Dr Jean Kaseya,” says Prof. Yap Boum, Deputy Manager at the Incident Management Support Team of Africa CDC.
“The continues decline in high burden countries is happening. However, Mpox remains quite active in some countries,” he stressed.
The ECG cited prevailing epidemiological data and challenges facing the continent wide response efforts to reach the decision. Specifically, the committee of experts cited continued presence of surge in cases, with new countries like Senegal, Gambia, Mozambique recording cases, while other countries are witnessing flare-ups, notably Guinea, Ghana, Liberia, and Zambia.
According to Prof. Yap, the committee is expected to reconvene in few weeks to decide on the way forward about the emergency situation.
In the meantime, the experts forwarded some recommendations the agency wants affected countries to focus on in the coming weeks, among these are mobilization of more vaccine doses and closing the testing coverage gap. The Africa CDC says 6.4 million more doses of vaccines are required for the continental response. With 3 million doses so far delivered to 12 countries, only one 1million doses have been administered.
Surveillance and cross border coordination are also considered key part of the ECG’s recommendations.
However, the continent made gains in laboratory testing, which increased from 30 percent in Week 33 to 66 percent in the week under review.
“This means that 7 out of 10 people suspected have been tested,” said Prof. Yap, citing the need to increase this to 100 percent coverage.
In spite of these, Africa CDC says there was a remarkable decline in cases across the continent. In Sierra Leone, this decline is attributed to the government’s intensified community surveillance campaign. This reduction in cases is supported by data for the test positivity rate, which stands as 51 percent, as at September 4.
Overall, Sierra Leone witnessed 85 percent reduction of cases from the peak period to date, the data shows.
“The transmission is low but it is persistent, which means that the hotspot containment and tight surveillance remain critical,” says Prof Yap.
The death among Mpox patients in Sierra Leone is found to be higher among people living with HIV, especially among those who aren’t under treatment, as well as people dealing with other comorbidities. This, says Prof. Yap, calls for prioritization of the healthcare needs of HIV positive people in the context of the Mpox response.
“Action is being taken to ensure that adequate care is provided to HIV positive patients to make them priority in terms of vaccination, but also to ensure that within the community the sensitization to avoid stigmatization is also implemented to allow people with HIV and any other conditions to seek care and to be confident about the capacity the system has to take care of them at the hospital,” Prof. Yap told journalists at the weekly press briefing of the Africa CDC on Thursday.
“That’s the only way we will prevent some flare-ups as we move toward the end of the outbreak,” he said.