By Kemo Cham
As countries race to contain spiraling cases of Mpox across Africa, some emerging realities of the virus have been keeping epidemiologists worried.
In Sierra Leone, the strain in transmission – clad 2b – has proven more virulent than was expected, resulting in a rare form of genital lesions in patients.
Sierra Leone is one of the last countries to fall to the ongoing global epidemic after recording its first case on 10th January, 2025. Three months later, it has recorded 588 cumulative confirmed cases and six deaths, as at April 24, according to data from the National Public Health Agency (NPHA).
Health authorities say majority of patients are presenting with advance form of lesion on their genital regions, which Dr Mustapha Jalloh, the Mpox response lead at the public health agency, described as serious. Dr Jalloh told reporters on Wednesday that genomic profiling of the virus revealed that some mutation was already occurring, which has made cases in the country different from what is seen in other countries.
“The level of virulent cases we are getting now…especially with genital lesions, both male and female…is serious,” he said at a press conference at the Emergency Operation Center of the Ministry of Health at Cockerill in Freetown.
“This is not what we thought of initially. If you go to hospitals today and see evidence of cases, it is really pathetic. People are suffering from this disease,” Dr Jalloh added.
Mpox, previously known as monkeypox, was first discovered as a zoonotic disease that causes fevers, headaches and boils. The virus also spreads from person to person, through close physical contacts.
But epidemiologists say the virus has exhibited new characteristics in the current epidemic, including its mode of transmission and symptoms, which call for concern.
First discovered among monkeys in a laboratory in Denmark in 1958, there have been numerous outbreaks of Mpox in human populations starting in 1970 in the Democratic Republic of Congo.
The most recent outbreak started in 2022, affecting over 120 countries, according to data from the World Health Organization (WHO).
Genomic sequencing has revealed the existence of multiple strains of the virus, divided into two main strains – Clade I and Clade II. These are further divided into Clad Ia and Clad Ib; Clad 2a and Clad 2b.
Clade I is known to be endemic to Central Africa and is considered more severe, as was seen in the DR Congo, which has been the epicentre of the current outbreak that began in late 2023. Clade 2 is endemic to West Africa and is generally considered less severe.
The 2022 outbreak, which started on May 6th with the first case in the UK, marked the first time Mpox cases were recorded in large numbers in non-endemic zones. Cases were recorded in Europe, North America and Australia. It was driven mainly by the clad 2 strain, believed to have originated in Nigeria. The transmission of the virus was largely associated with sexual activities among people engaging in same sex relationships.
On July 23rd, 2022, WHO declared the outbreak a Public Health Emergency of International Concern (PHEIC), under the 2005 International Health Regulations (IHR) — the global health agency’s highest-level alert. The emergency was declared over on May 11th, 2023, after over 100, 000 confirmed cases and over 200 deaths.
Cases continued in smaller numbers, until an outbreak of a new strain – Clad 1b – in DR Congo in September 2023. On August 13th, 2024, the Africa Centers for Disease Control and Prevention (Africa CDC) declared the new outbreak a Public Health Emergency of Continental Security, after cases escalated across the continent. WHO followed suit by declaring it PHEIC for the second time within two years.
According to the NPHA, genome sequencing revealed that the Mpox strain in Sierra Leone has been circulating in the country since 2022.
According to the analysis, the country had its first ever case of the virus in 1994, an imported case from Cote d’Ivoire. In 2002, it was exported to Nigeria. And in 2021 it was reintroduced in Sierra Leone.
“Since then, it has been circulating in the country…” said Dr Jalloh.
In the first two months of recording the first case in January, patients have been presenting with mild symptoms, until cases suddenly surged in early April, according to the agency. As of April 17th, 95 percent of cases appeared with genital lesions, it said.
Another question raised by Clade 2b in this transmission is that while the strain was previously known to mainly transmit through close physical contact, in Sierra Leone over 80 percent of cases have been found to have no epidemiological link to existing cases. And according to the public health agency, 100 percent of the patients had no travel history, which it says further proves that the virus has been circulating in the communities long before it was detected at the beginning of the year.
Prof. Foday Sahr, Executive Director of NPHA, however warns that regardless of the strain, Mpox poses a great danger to patients with pre-existing diseases and immunosuppressed conditions. He noted that all four people who had died from the virus in the country as at April 17th, had at least one such pre-existing diseases.
“In 1994, it (Mpox) was gotten from animals, now it is from humans to humans. It is a new disease, so people need to know the reality,” Prof. Sahr said at a special briefing for bloggers earlier in the week.
Another thing of interest to the NPHA, according to the public health agency boss, is the fate of recovered patients. He said there have been no idea what happens to the people who had so far recovered from the disease.
“We want to know what happens to those who recover after six months, after one year… We want to follow them through. It is a new disease with a lot of unknowns,” he said.
Meanwhile, the agency is intensifying its response measures through surveillance and vaccination. In collaboration with the Ministry of Health, it launched a nationwide vaccination drive in March, specifically targeting most at risk populations like health workers and contacts of infected persons. Priority is given to people above 12 years, excluding pregnant women and lactating mothers.
Dr Desmond Maada Kangbai, head of the Expanded Programme on Immunization at the Ministry of Health, said because of the limited available doses of the vaccine, they are focusing on those at highest risk of contracting the virus, especially healthcare workers who are crucial to maintaining service delivery in health facilities.
“If we start having cases among healthcare workers there will be a break in service delivery (and) you may go to some health facilities and you would not see healthcare workers. We don’t want that to happen like in Ebola,” he said.
The Mpox response lead, Dr Jalloh, stresses the importance of vaccination in efforts to prevent prolongation of the outbreak.
“What we saw in our genomic profiling was that the virus would continue spreading until 2028 if we don’t take the appropriate measures,” he said.
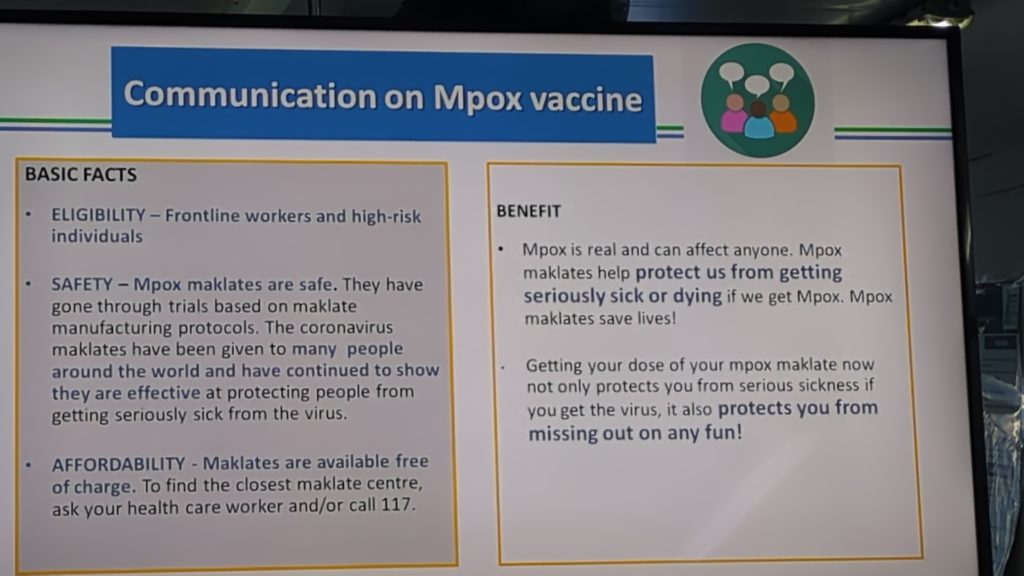
But a major challenge for the health authorities remains as to how to prioritize the available vaccines in the face escalating cases and number of contacts.
“All is not lost,” says Harold Thomas, Risk Communication expert. He notes that besides vaccination, Mpox has a lot of other preventive measures that are non-pharmaceutical interventions, like infection prevention control.
But as risk communication lead, Thomas is concerned about denial of the existence of the virus through mis and disinformation on and offline.
“We don’t want it to cause a lot of problem before we believe,” he says, stressing the significance of people adhering to these “cheaper” preventive measures.