By Kemo Cham

at the Radisson Blu Mammy Yoko Hotel in Abdeen.
Image, Morrie Koroma, ManoReporters.
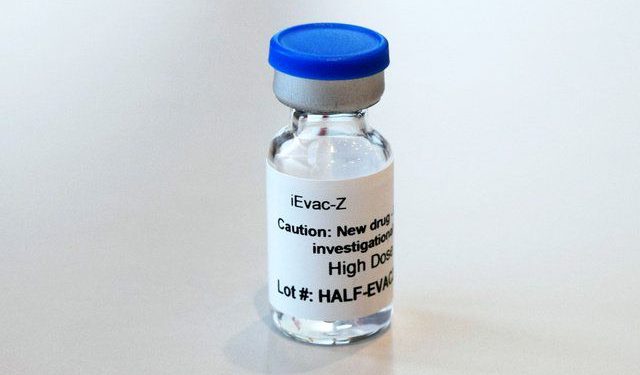
An experimental Ebola vaccine co-developed by one of the world’s leading virologists is set for trial in Sierra Leone.
The novel iEVac-Z is inactivated vaccine, a modified Ebola virus grown under regular laboratory condition. It was first trialed in Japan in 2019.
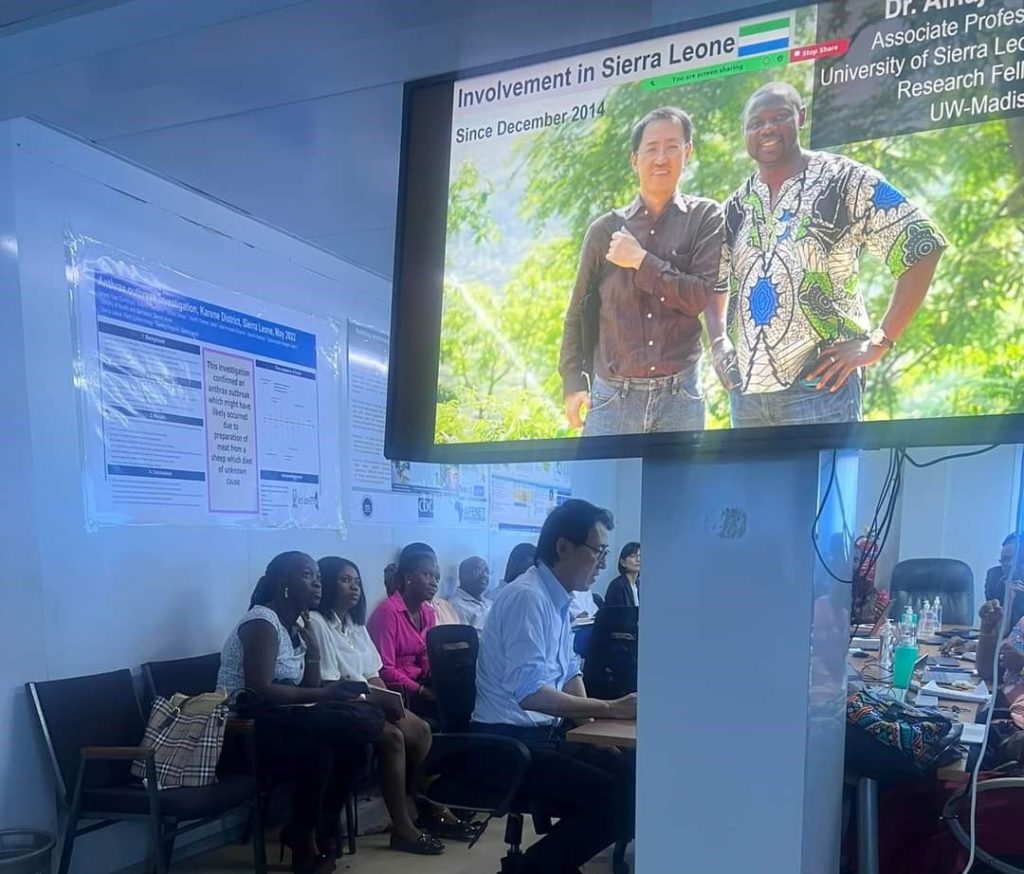
Yoshihiro Kawaoka, professor of pathobiological sciences at the University of Wisconsin – Madison School of Veterinary Medicine, who co-created the vaccine, is working alongside his long term Sierra Leonean collaborator Dr Alhaji Umar Njai to conduct another trial phase in the country.
Prof. Kawaoka was in Sierra Leone in June and met authorities and potential partners for the next phase of his research. He told ManoReporters that the Sierra Leone trial is important in that it would be the first to be done in a country that has had Ebola outbreak experience.

Sierra Leone and its Mano River Union neighbours Guinea and Liberia witnessed the world’s deadliest outbreak of the Ebola Virus Disease (EVD) between 2013 and 2016, which became known as the West African Ebola epidemic. It started in Guinea and spread to other countries and later been declared by the World Health Organization (WHO) as a global international public health emergency.
A total of 28,616 cases were reported in the three countries, with 11,310 deaths, according to data from the World Health Organization (WHO).
Sierra Leone had the highest number of cases – 14,124, with 3,956 deaths.
Prof. Kawaoka worked in the country during that epidemic. But his work then focused on survivors of the deadly hemorrhagic fever disease. Through their study, he said, they sought to understand why some people were dying and others were recovering from the disease.
Blood samples from survivors were compared and their molecules identified, enabling the researchers to tell whether the patient would survive or die.
“Analysing this information, you can tell who may die and so you can put more resources into saving that person’s life,” the virologist said.
“What we learnt here may not directly translate to vaccine development, because it’s a different area, but still, we made the vaccine and we tested it in Japanese population. It’s safe. So, the next step would be to come to a host country to repeat the same experiment,” he added.

Prof. Kawaoka’s work on viruses however started long before that.
Besides Ebola, he is perhaps best known for his work on the Influenza virus. He created a new influenza virus from DNA sequence, with which a live attenuated vaccine currently in used in Europe and the US was developed.
According to Kawaoka, his work on the Ebola vaccine was based on animal models, making the Sierra Leone trial important because of the country’s experience with the virus.
“One reason why Sierra Leone testing is important is because this would be the country were Ebola virus may cause problem. It is highly unlikely that Japanese population may encounter Ebola outbreak. So I think it’s important for us to do the clinical trial in this country and then go to the next level,” he said.
Prof. Kawaoka and his colleagues plan to advance infectious disease research through Sierra Leone, Japan and United States collaboration. They also intend to conduct additional immunological studies on EVD survivors to understand antibody memory, expand their studies on other infectious diseases, build local capacity through an infectious disease research training program and center. While in Freetown, his team met with the leadership of the Ministry of Health and other relevant ministries, as well bodies like the Pharmacy Board, Ethics Committee, Sierra Leone Association of Ebola Survivors and University of Sierra Leone to discuss these.
The West African Ebola epidemic spurred huge interest in the development of a vaccine and some of the vaccines that were eventually approved were trialled in Sierra Leone, including the Strive, Ebovac and Johnson and Johnson vaccines.
Dr Njai, himself an alumni of the University of Wisconsi, participated in the development of some of those vaccines. He said trialling the novel iEVac-Z Ebola vaccine in Sierra Leone has numerous significance for the country, noting that the world needs a diverse array of vaccines in the market that can be utilized against any other outbreak anywhere.
Since the West African outbreak, there have been five other outbreaks, including in Guinea. The Democratic Republic of Congo alone battled about three outbreaks. The most recent outbreak was in Uganda, which was declared over in 2023.
Vaccines are usually designed to target specific strains of a virus, and much of the existing vaccines are for the predominant Zaire strain responsible for the West African outbreak. The Sudan strain, which was responsible for the Ugandan outbreak, has no targeted vaccine yet. Dr Njai said this makes it important to create as many vaccines as possible that can deal with all strains.
“We need to be better prepared both in our offense and in our defence against these pathogens,” he said.
Another significant thing about the Kawaoka vaccine, according to Dr Njai, is that it will be a little cheaper and cost effective than existing vaccines. He said data from previous trials also shows that it is more effective compared to approved vaccines.
“So, combination of the fact that it has better efficacy, it is safe and it will be cheaper, makes it more affordable to people in developing countries, including Sierra Leone,” he said.
Dr Njai said trialling the vaccine in Sierra Leone also puts the country on leadership and priority positions. He explained that during the Covid-19 pandemic, the distribution and supply of vaccines largely favoured countries where those vaccines had been developed or where they had ownership over them.
“I think Sierra Leone participating in this one and also having a Sierra Leonean as part of the team, is also important in making us in the drivers’ seat.
“Sierra Leoneans participating in it means that we are able to capture the genotypes of the various people in the country. That will put the country in a better position in terms of its effectiveness,” he said.