Collaborative approach is the only way to tackle cervical cancer, experts and campaigners have said and reiterated the need for more public awareness on the leading killer cancer disease in Sierra Leone.
Official data indicate a rising trend of cancers generally and cervical cancer in particular in the country. This was the subject of discussion by a panel of experts in Freetown on Tuesday, February 7, as part of commemoration of World Cancer Day, which officially falls on February 4th.
Cancer is an uncontrolled growth of abnormal cells. The part of the body the growth occurs determines the type of cancer, which include lung cancer, breast cancer and cervical cancer.
World Health Organization (WHO) data show that Cervical Cancer is the fourth most common cancer globally, with about 600, 000 annual cases. In Sub Saharan Africa, which accounts for around 85 percent of the global disease burden, cervical cancer is the second most common cancer and the one responsible for the highest number of deaths, with 117, 316 yearly cases.
The situation in Sierra Leone reflects this sub regional reality. Figures from the national Cancer Registry indicate that even though Cervical Cancer is the second largest (after Breast Cancer), it’s the biggest killer of all cancers among women aged between 14 and 44. It also shows that 500 cases are recorded annually, with an estimated 400 of the victims dying due to the disease.
Tuesday’s event, organized by the Well Woman Clinic1, in collaboration with the US-based pharmaceutical technology firm, VARIAN, provided a platform for experts and campaigners to share ideas on tackling what has been described as a silent killer.
The almost four-hour long session began with the screening of a film depicting the impact of cervical cancer and efforts to eliminate it globally. The documentary explores the realities of people living with the disease in three countries on three different continents – Australia, Malaysia and Zambia. It exposes how the condition destroys marriages and affect women’s employability, with significant mental health implications on whole families.
Dr. Stephen Mupeta, a reproductive health expert, said that cervical cancer requires the same multisectoral approach that was used to deal with the HIV pandemic.

Cervical cancer affects the cervix. Therefore, it is a disease of women. It is caused by several means, but the most common one is the Human Papilloma Virus (HPV), which is transmitted through sexual intercourse. Smoking is also a high risk factor, and people who are chronically immunocompromised are also at risk of contracting it.
The good news is that cervical cancer is preventable, through vaccination. It is one of the cancers that can be easily detected in advance due to how the cells changes. But through regular screening, it is possible to prevent it before the cells become cancerous.
HPV can go unnoticed for decades before cancer develops, at which point it may be too difficult to control.
Experts say at least half of sexually active people will have HPV at some point in their lives, but few women will get cervical cancer. While some HPV types can cause changes on a woman’s cervix that can lead to the disease over time, other types can cause genital or skin warts. This is why it is important to undertake regular screening, to rule out any chance of the cancerous cells developing.
However, the nature of the condition makes it difficult for many women to discuss it, leading to many dying in silence.
Campaigners say easy access to antibiotics means that women can go and get it when they feel unwell. And because symptoms sometimes associated with cervical cancer are similar to those of many other sexually transmitted diseases, someone infected with cervical cancer can continue taking these antibiotics until it’s too late.
Global targets
The global target of elimination of Cervical Cancer strategy envisages that all countries must reach and maintain an incidence rate of below four per 100, 000 women. Achieving that goal hinges on three key pillars. These are to fully vaccinate 90% of girls with the HPV vaccine by the age of 15; screening 70% of women using a high-performance test by the age of 35, and again by the age of 45; and treating 90% of women with pre-cancer and managing 90% of those with invasive cancer.
Each country is expected to meet the 90-70-90 targets by 2030 to get on the path to eliminate cervical cancer.
And for this to be realized, Dr Mupeta, who is the Technical Specialist on Maternal Health and Family Planning at the United Nations Population Fund (UNFPA) in Sierra Leone, stressed the need for collaboration and awareness raising.
“You cannot eliminate any disease by sticking to yourself. Multisectoral collaboration is very critical,” he said.
A Zambian national, Mupeta was training in his specialty area when his country started its Cervical cancer programme in 2006. He believes that Sierra Leone is in a better position than Zambia when the southern African nation started its campaign.
The HPV vaccine has been available in most developed countries for about two decades now. Gavi, the Vaccine Alliance and its partners, are now working to ensure it is available to lower income countries.
Through this support, Sierra Leone became the 19th African country to introduce the vaccine in October 2022. Over 150,000 girls aged between 10 and 15 across the country were targeted with the vaccine that is administered in two doses.
Those who were vaccinated are expected to get their second dose by April this year.
People with multiple sexual partners are highly prone to cervical cancer. For this reason, some campaigners are calling for the vaccination of boys. But with little resources, the government is focusing on girls, even within a limited age bracket.
The plan, according to officials in the Expanded Programme on Immunization (EPI) in the Ministry of Health, is to make the vaccine available to girls aged 9–15 from 2023 onwards.
See and treat
The introduction of the HPV vaccine in Sierra Leone and subsequent inclusion into the routine immunization system followed several months of planning, after a 2014 Gavi-supported pilot vaccination scheme undertaken in the southern Bo District. The Ebola Virus Disease and COVID-19 outbreaks led to repeated postponement of the introduction.
Sierra Leone, with the help of WHO and other partners, has also rolled out trainings for health workers across the country on the diagnosis and treatment of cervical cancer. Some 50 people were trained on how to screen and treat cases, in line with WHO’s recommended ‘see and treat’ approach.
As part of this programme, 476 women were screened and 62 were found to be positive; about 15 received surgery.
“This tells us a lot needs to be done,” says Binyam Hailu, Maternal and Child Health Officer at the WHO Country Office in Freetown.
“We have every district hospital offering screening service. What we need now is dissemination of information,” he added.
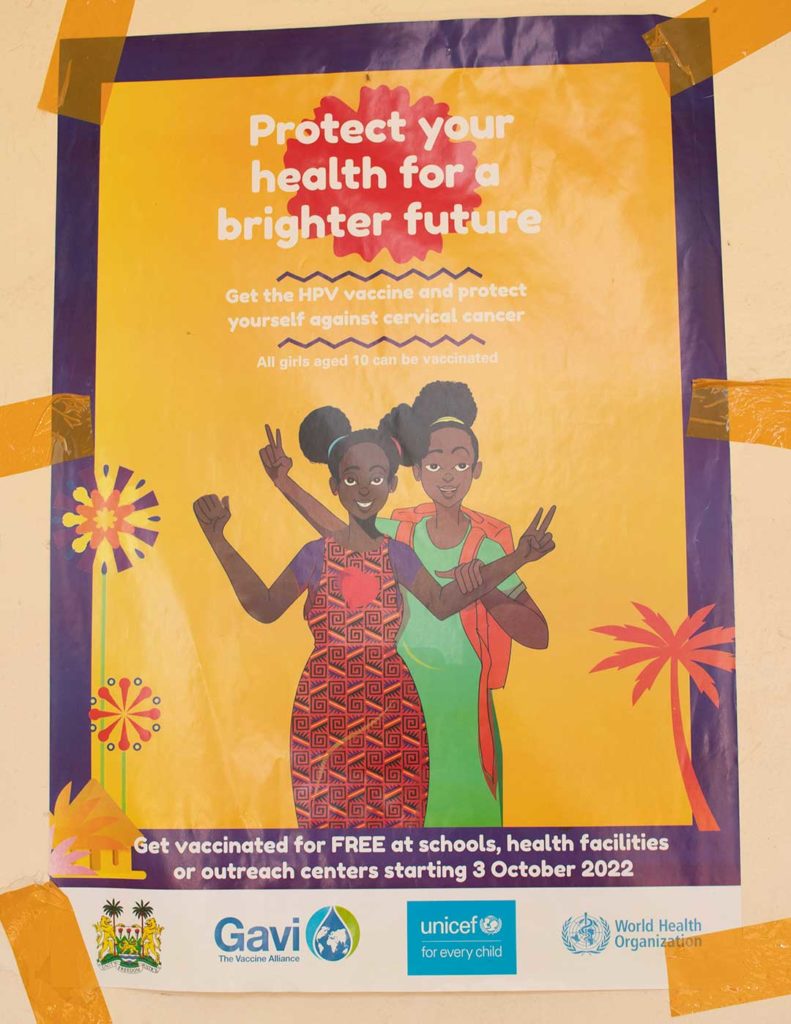
A poster on a school wall in Freetown, part of the government’s communications campaign to drive uptake of the HPV vaccine. Photo credit, WHO Sierra Leone
The government, in 2021, also launched a Public-Private Partnership Pilot Programme on Cervical Cancer Screening, in collaboration with the University of Sierra Leone Teaching Hospitals Complex (USLTHC), Well Woman Clinic and Ramsy Medical Laboratories. That initiative, spearheaded by UNFPA, was made possible thanks to funding under a China South-South Cooperation project designed to improve women’s health and reaching vulnerable and marginalised women at high risk of maternal mortality and cervical cancer. Nine healthcare facilities nationwide are being supported under this scheme.
In addition, it has resulted in the development of three key national documents, namely, the first ever National Policy on Cervical Cancer, a Strategic Plan, and Clinical Guidelines for the management of cervical cancer.
Another partner helping the government’s response to cervical cancer is World Hope International (WHI), which in 2022 launched Sierra Leone’s first district-wide screening initiative in the northern Bombali District. It trained a small team of nurses and midwives in the “See-and-Treat” method.
By the end of 2022, WHI had screened over 2,000 women. Up to 10% of them needed treatment, and 90% received it the same day.
The gold standard for Cervical Cancer screening is the PAP test, but it’s expensive. Most countries therefore go for the WHO recommended simple and inexpensive Visual Inspection and Acetic Acid (VIA) test. The results of a VIA test are immediately available and do not require any laboratory support.
Histopathologist Prof. Babatunde Duduyemi argued in favour of the PAP test, noting that Sierra Leone now has at least two pathologists who can read PAPs smears. The Consultant at the University of Sierra Leone Teaching Hospitals Complex has been involved with diagnostics efforts of cancer in the country since 2021.
“The advantage is that you are seeing the cells with microscope. This is the most advanced form of the testing. If the virus is detected, it can be treated and prevented,” he said.
One thing all these experts agree on is that early detection is also very important for Sierra Leone, a country that doesn’t have radiotherapy, which is required in dealing with advance cancer stages.
And for early detection to take a foothold, the country must overcome the hurdle of silence due to shame associated with cervical cancer, said Dr Isaac Small.
“Cervical cancer is not like breast cancer. It is difficult to talk about. For most women, discussing private parts is a taboo. So, our focus should be how to break that taboo,” said Dr Small, who is leading the country’s newly established Onchology unit within the main referral hospital of Connaught.
The unit started as a clinic in 2017 to provide not just surgical services but also chemotherapy and palliative care. Dr Small benefitted from a training in Egypt which enabled him to spearhead this initiative.
“Regardless of what you do, without a developed cancer programme, without sensitization, you will still be dealing with end stage cases,” he said.